Arizona’s desert climate presents unique challenges and opportunities for people living with chronic pain. The CDC reported in 2024 that approximately 51.6 million American adults experience chronic pain, affecting daily activities and quality of life. For Arizona residents, understanding how extreme heat, dramatic barometric pressure changes during monsoon season, and rapid temperature fluctuations affect pain allows for better management strategies.
Arizona Pain and Spine Institute serves Cave Creek, Scottsdale, Phoenix, and surrounding Valley communities with pain management protocols specifically designed for desert living. This comprehensive guide explains evidence-based approaches to pain relief, Arizona-specific environmental factors, and how multimodal treatment helps patients achieve lasting improvement while enjoying the Valley’s active lifestyle.
Understanding Chronic Pain in the Arizona Context
Chronic pain is defined as pain lasting more than three months. The 2022 CDC Clinical Practice Guideline explains that chronic pain differs from acute pain in its duration, causes, and treatment requirements. While acute pain serves as a protective warning signal, chronic pain involves complex changes in the nervous system that require comprehensive management approaches.
For Arizona residents, chronic pain manifests against the backdrop of unique environmental factors. Dr. Dan Ryklin of Arizona Pain and Spine Institute has extensively studied how Arizona’s climate patterns affect pain conditions. “People move to Arizona expecting consistent, dry weather to help their pain,” explains Dr. Ryklin. “What they don’t realize is that our monsoon season creates more dramatic atmospheric changes than many other climates. We can go from 10% to 60% humidity in hours. That kind of rapid shift affects sensitive pain conditions.”
Research published in a 2025 PMC review titled “Weathering the Pain” documented that ambient temperature plays a significant role in chronic pain syndromes. Temperature changes can impact endogenous opioid release, affect ion channels on primary afferent nerves, alter local cytokine release, and change overall nerve function. These mechanisms explain why Arizona patients experience predictable pain pattern changes with seasonal shifts.
Get Back Your Normal Life Again
As pain specialists, we can guarantee that we are more than qualified in alleviating your pain and treating your condition.
The Arthritis Foundation identifies Arizona as one of the ideal states for joint pain sufferers due to the dry, warm climate. However, this doesn’t mean pain disappears automatically. Instead, understanding and working with Arizona’s climate allows for optimized pain management strategies.
How Arizona’s Unique Climate Affects Different Pain Conditions
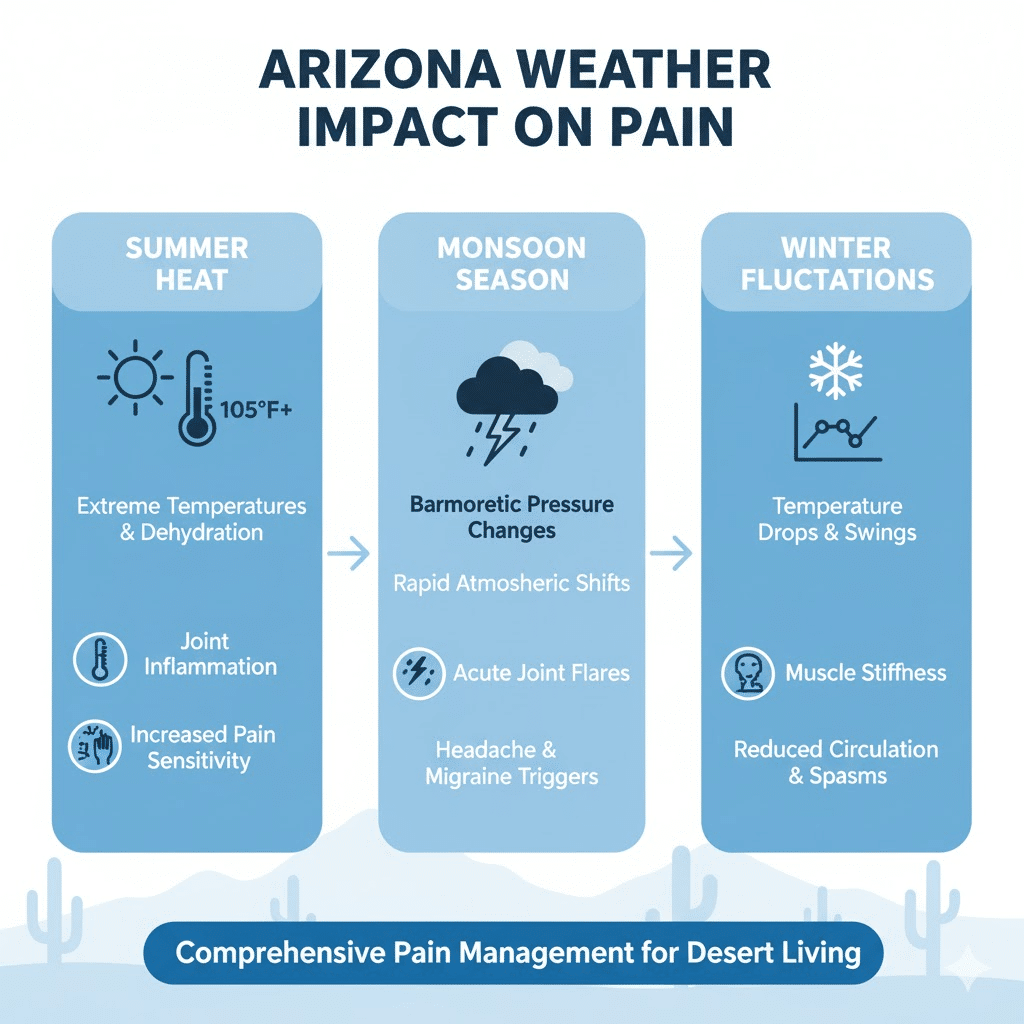
Each Arizona season creates specific challenges that Arizona Pain and Spine Institute addresses through tailored treatment protocols.
Summer Heat and Inflammation
When temperatures consistently exceed 105 degrees from June through September, Dr. Navdeep Khan notes increased cases of heat-related inflammation among patients from Gilbert, Chandler, Cave Creek, and other Valley communities. Higher temperatures can lead to increased inflammatory responses in the body, particularly affecting arthritis patients where inflammation already plays a significant role in pain.
Dehydration during Arizona summers presents another challenge. Research from Orthopedic Sports Therapy shows that when the body loses just 2% of water, cerebrospinal fluid volume decreases by 10%. Cerebrospinal fluid provides shock absorption to the spine and acts as a brain cushion. Reduced CSF leads to poor repair, decreased healing of structures, and toxin buildup—all of which increase pain.
Arizona Pain and Spine Institute recommends that summer pain management include hydration strategies, modified activity timing (early morning or evening outdoor activities), and indoor exercise alternatives during peak heat hours. For patients with conditions like fibromyalgia or complex regional pain syndrome, sun exposure itself can trigger pain flares, requiring protective measures including lightweight clothing, hats, and sunscreen.
Monsoon Season Barometric Pressure Changes
Arizona’s monsoon season from July through September brings dramatic barometric pressure shifts that significantly affect pain patients. During monsoon storms, barometric pressure in the Phoenix area can drop 20-30 millibars in just hours—one of the most dramatic shifts in the continental United States.
Dr. Ryklin explains that these sudden pressure changes trigger intense pain flares in patients with arthritis and fibromyalgia. Medical theories suggest that pressure drops increase the amount of pressure on joints. Changes in barometric pressure also affect individuals with chronic headaches and can lead to increased joint pain throughout the body.
Arizona Pain and Spine Institute’s approach to monsoon-season pain includes proactive treatment strategies implemented before the season begins. Rather than reactive pain management after flares occur, the practice helps patients prepare their bodies to handle pressure changes more effectively. This may include optimizing anti-inflammatory protocols, ensuring proper hydration status, and having interventional procedures completed before monsoon season intensifies symptoms.
Winter Temperature Fluctuations
While Arizona winters remain mild compared to northern climates, dramatic daily temperature swings—sometimes 30 degrees in a single day—affect pain conditions. Dr. Ryklin notes that these fluctuations impact everything from arthritis to neuropathy.
Research shows that cold temperatures cause blood vessels to constrict to preserve heat, reducing circulation to muscles and joints. Decreased blood flow leads to stiffness and makes movement more painful. Additionally, muscles contract in colder temperatures, increasing tension and discomfort. For Arizona residents accustomed to consistent warmth, even mild winter cold can trigger pain responses.
Haven Health research on Arizona seniors found that while Arizona’s climate is generally ideal for joint health, the impact of seasonal changes still requires management strategies. The key is recognizing that even in paradise, seasonal variations affect pain and preparing accordingly.
Low Humidity Benefits
Arizona’s consistently low humidity (typically 10-30% versus 60-80% in humid climates) provides genuine benefits for most pain conditions. High humidity can increase joint inflammation and aggravate conditions like rheumatoid arthritis and fibromyalgia. The dry desert air allows for better joint function and reduced inflammation for many patients.
However, low humidity also requires diligent hydration to prevent dehydration-related pain increases. Arizona Pain and Spine Institute educates patients about balancing the benefits of dry air with proper hydration protocols throughout the year.
Arizona Pain and Spine Institute’s Comprehensive Evaluation Process
Effective pain management begins with thorough understanding of each patient’s specific condition, lifestyle factors, and goals. Arizona Pain and Spine Institute’s evaluation process addresses both medical complexity and Arizona-specific considerations.
Initial Consultation and Pain Assessment
The evaluation starts with an extensive consultation reviewing medical history, previous treatments, current medications, and how pain affects daily activities. For Arizona patients, this includes discussing activity patterns—do they golf regularly in Scottsdale, hike the Superstition Mountains, maintain pool-based exercise routines, or work in outdoor environments?
Understanding lifestyle allows physicians to develop practical treatment plans that fit how patients actually live. A retiree who golfs three times weekly requires different pain management strategies than a construction worker exposed to summer heat or an office professional sitting at a desk in air conditioning.
The American Chronic Pain Association-Stanford Resource Guide emphasizes that successful pain treatment means learning to independently self-manage conditions in ways that allow life to continue, maximizing participation in everyday activities. Arizona Pain and Spine Institute adopts this philosophy, recognizing that patients are active participants in their recovery rather than passive recipients of treatment.
Functional Assessment and Physical Examination
Beyond identifying pain locations, Arizona Pain and Spine Institute assesses how pain affects function. Physicians evaluate range of motion, strength, flexibility, and pain patterns during specific movements. This functional assessment reveals limitations that impact quality of life and identifies treatment targets.
For example, a patient whose knee pain prevents morning desert walks has different functional goals than someone whose shoulder pain limits golf swings. The evaluation identifies these specific functional deficits and establishes measurable improvement goals.
Diagnostic Imaging Review
When appropriate, Arizona Pain and Spine Institute reviews or orders diagnostic imaging including X-rays, MRIs, or CT scans. These studies reveal structural problems such as arthritis severity, disc degeneration, ligament tears, or nerve compression. Understanding structural pathology helps determine which treatments will most effectively address underlying problems.
The 2024 Reed Group Chronic Pain Guidelines emphasize that diagnostic procedures should identify clinical pathology and guide treatment selection. Imaging serves this purpose when used appropriately to inform treatment planning rather than as routine screening.
Pain Pattern Analysis and Triggers
Arizona Pain and Spine Institute maps each patient’s pain patterns, including when pain worsens, what activities aggravate symptoms, and whether Arizona’s seasonal changes trigger flares. This detailed analysis reveals treatment opportunities and helps patients understand their pain better.
For patients who report monsoon-season flares, treatment planning might include proactive interventional procedures before July. For those whose pain worsens with summer heat, protocols emphasize indoor exercise options and hydration strategies implemented before temperatures peak.
Multimodal Pain Management: The Arizona Pain and Spine Institute Approach
The 2022 CDC Guideline and 2024 Stanford-ACPA Resource Guide both emphasize that multimodal treatment produces superior outcomes compared to single-intervention approaches. Arizona Pain and Spine Institute applies this evidence-based principle through comprehensive treatment plans addressing pain from multiple angles simultaneously.
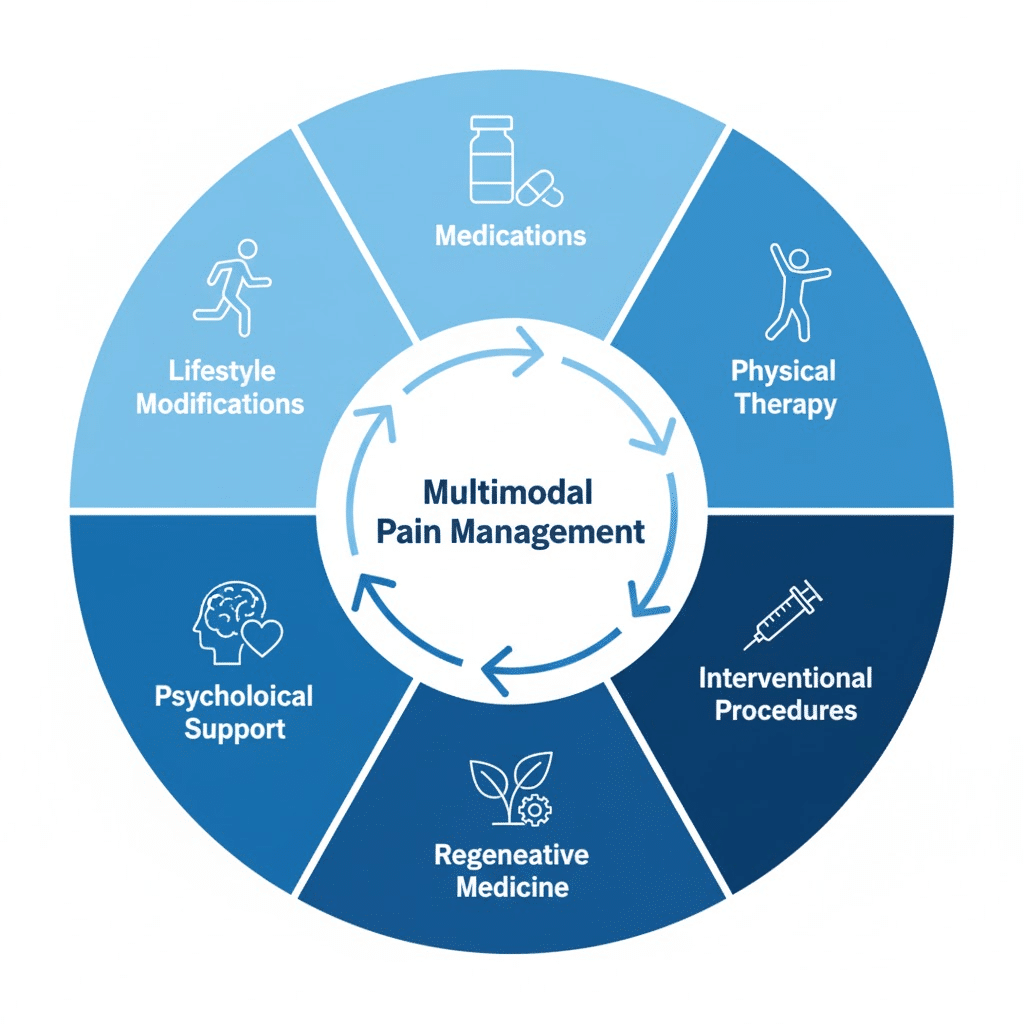
Non-Opioid Medication Management
Pain specialists generally recommend non-opioid medications as first-line pharmaceutical interventions. Arizona Pain and Spine Institute’s approach to medication management emphasizes options with favorable benefit-risk profiles.
Non-steroidal anti-inflammatory drugs (NSAIDs) reduce inflammation and pain for many musculoskeletal conditions. However, long-term NSAID use requires monitoring for gastrointestinal and cardiovascular effects. Physicians work with patients to find lowest effective doses and implement protective strategies when appropriate.
Neuropathic pain medications including certain antidepressants (amitriptyline, duloxetine) and antiepileptic drugs (gabapentin, pregabalin) address nerve-related pain more effectively than traditional pain relievers. These medications modulate how nerves transmit pain signals rather than simply masking symptoms.
Topical medications applied directly to painful areas provide localized relief without systemic side effects. Options include lidocaine patches, diclofenac gel, and capsaicin creams. For Arizona patients concerned about medication side effects, topical approaches offer alternatives worth exploring.
The WHO 2023 guideline on chronic low back pain reinforces patient-centered approaches prioritizing safety. Arizona Pain and Spine Institute follows this principle by individualizing medication selection based on each patient’s specific condition, other health factors, and personal preferences.
Physical Therapy and Exercise Medicine
Regular physical activity tailored to individual capabilities improves pain, function, and quality of life according to multiple clinical guidelines. Arizona Pain and Spine Institute coordinates with physical therapists to develop Arizona-appropriate exercise programs.
Summer exercise protocols emphasize pool-based activities that combine therapeutic benefits with cooling effects. Swimming and water aerobics provide low-impact cardiovascular exercise and resistance training while preventing overheating. Many Arizona communities offer accessible pools year-round.
Fall and winter enable outdoor activities during Arizona’s most pleasant weather. Desert hiking, walking trails through Scottsdale or Cave Creek, and outdoor yoga capitalize on mild temperatures while building strength and flexibility. Arizona Pain and Spine Institute helps patients transition between seasonal activity options while maintaining consistent exercise routines.
Spring golf season presents opportunities and challenges. Golf involves rotational movements that can stress the spine and joints. Dr. Ryklin has developed season-specific protocols accounting for golf-related strain patterns common in Mesa and Scottsdale communities. Proper warm-up routines, technique modifications, and complementary strengthening exercises help golfers manage pain while enjoying the sport.
Motor control exercises, tai chi, and yoga all demonstrate benefits for chronic pain according to evidence reviews. These practices combine physical movement with mental focus, addressing both physical and psychological pain components. Arizona’s abundant yoga studios and tai chi classes make these modalities accessible to Valley residents.
Interventional Pain Procedures
When conservative treatments provide insufficient relief, interventional procedures target specific pain generators with precision. Arizona Pain and Spine Institute offers multiple interventional options tailored to different conditions.
Epidural steroid injections deliver anti-inflammatory medication directly to irritated nerve roots in the spine. These injections benefit patients with radiculopathy—pain radiating down arms or legs from spinal nerve compression. The 2024 NIA Clinical Guidelines specify appropriate use criteria ensuring patients receive interventions when evidence supports benefit.
Facet joint injections address pain originating from small joints connecting vertebrae. These joints can develop arthritis and cause localized back or neck pain. Injections provide diagnostic information (confirming the facet joints as pain sources) and therapeutic benefit through anti-inflammatory effects.
Radiofrequency ablation (RFA) uses controlled heat to interrupt pain signals from specific nerves. Dr. Ryklin notes that for many monsoon pain sufferers, RFA proves “nothing short of miraculous.” The procedure essentially installs a circuit breaker between weather-sensitive areas and the brain’s pain centers. Effects typically last 6-12 months, after which treatment can be repeated if needed.
Nerve blocks target peripheral nerves causing localized pain. Whether addressing shoulder pain, hip discomfort, or facial pain syndromes, precisely delivered nerve blocks can provide substantial relief. These procedures use ultrasound or fluoroscopic guidance ensuring accurate medication placement.
Spinal cord stimulation represents an advanced option for patients with persistent nerve pain unresponsive to other treatments. Small electrodes placed near the spinal cord deliver mild electrical signals that alter how pain messages reach the brain. The 2024 Neurostimulation Appropriateness Consensus Committee provides surgical technique recommendations that Arizona Pain and Spine Institute follows.
Regenerative Medicine Therapies
Regenerative medicine harnesses the body’s natural healing mechanisms to repair damaged tissues. Arizona Pain and Spine Institute offers several regenerative approaches.
Platelet-rich plasma (PRP) therapy concentrates growth factors from the patient’s own blood and injects them into injured tissues. PRP has shown benefits for tendon problems, mild to moderate arthritis, and ligament injuries. The concentrated growth factors stimulate tissue repair and reduce inflammation.
Amniotic stem cell therapy, discussed extensively in Arizona Pain and Spine Institute’s regenerative medicine protocols, provides multipotent cells capable of differentiating into multiple tissue types needed for healing. The cells’ immune privilege and high growth factor content make them particularly effective for joint and soft tissue regeneration.
Prolotherapy involves injecting solutions that trigger controlled inflammation, stimulating the body’s healing response in chronically injured ligaments or tendons. This technique particularly benefits patients with joint instability from ligament laxity.
The advantage of regenerative approaches is addressing underlying tissue damage rather than simply managing symptoms. While not appropriate for all conditions, regenerative medicine offers genuine repair potential for properly selected patients.
Psychological Support and Cognitive Behavioral Approaches
Chronic pain involves psychological and emotional components alongside physical pathology. The VA/DoD 2022 Clinical Practice Guideline emphasizes addressing pain holistically, prioritizing whole-person care that considers psychological health, function, and quality of life.
Cognitive Behavioral Therapy (CBT) helps patients reframe pain-related thoughts, reduce distress, and improve coping strategies. Research consistently shows CBT improves outcomes for chronic pain patients. Rather than changing the pain itself, CBT changes how patients relate to and manage their pain experience.
Acceptance and Commitment Therapy (ACT) teaches patients to accept pain rather than constantly fighting it, while committing to actions aligned with personal values despite pain. This approach reduces suffering even when pain persists.
Stress management techniques including relaxation training, mindfulness meditation, and breathing exercises help reduce pain perception and improve overall wellbeing. Arizona Pain and Spine Institute incorporates these approaches as part of comprehensive care rather than treating them as separate from medical treatment.
For Arizona residents, managing pain-related anxiety about seasonal triggers (will monsoon season make pain unbearable?) becomes part of psychological support. Understanding that treatment plans account for seasonal variations reduces anticipatory anxiety.
Lifestyle Modifications for Arizona Living
Beyond specific medical interventions, lifestyle factors significantly impact pain management success in Arizona.
Hydration protocols adapted to desert living prevent dehydration-related pain increases. Arizona Pain and Spine Institute provides specific hydration recommendations based on individual activity levels and the season. During summer months, patients may need to double their usual water intake to maintain proper hydration.
Sleep optimization improves pain outcomes. Bodies use sleep to recover and prepare for the next day. For patients with chronic pain, sleep disturbances often worsen symptoms. Establishing consistent sleep schedules, creating cool sleeping environments (critical during Arizona summers), and addressing sleep disorders improves pain management outcomes.
Nutrition strategies support tissue health and reduce systemic inflammation. Anti-inflammatory dietary patterns emphasizing whole foods, omega-3 fatty acids, and colorful vegetables help manage pain. Arizona’s year-round farmers’ markets provide access to fresh produce supporting healthy nutrition.
Activity pacing prevents overexertion while maintaining function. Arizona’s pleasant fall, winter, and spring weather tempts patients to overdo activities after surviving summer heat. Proper pacing allows participation in desired activities without triggering pain flares.
Stress management addresses how psychological stress amplifies pain perception. Arizona’s lifestyle opportunities—from peaceful desert sunsets to outdoor recreation—can support stress reduction when patients make time for these restorative activities.
Specific Pain Conditions and Arizona-Optimized Treatment
Arizona Pain and Spine Institute treats multiple pain conditions with protocols accounting for desert living.
Chronic Low Back Pain
The 2021 Journal of Orthopedic & Sports Physical Therapy guidelines recommend multimodal treatment combining exercise, manual therapy, and education. Arizona Pain and Spine Institute follows this approach while addressing Arizona-specific factors.
Pool exercises provide excellent low-impact options for back pain patients during Arizona summers. The buoyancy reduces spinal loading while water resistance builds core strength. Year-round pool access in most Valley communities makes this consistently available.
For back pain related to disc problems or spinal stenosis, epidural steroid injections provide targeted anti-inflammatory treatment. When combined with physical therapy emphasizing core stabilization and proper movement mechanics, patients often achieve substantial functional improvement.
Arthritis and Joint Pain
Arizona’s dry climate provides genuine benefits for most arthritis patients. However, managing summer heat and monsoon pressure changes requires specific strategies.
Viscosupplementation injections deliver hyaluronic acid into arthritic knees, improving joint lubrication and reducing pain. This works particularly well for patients who want to maintain active Arizona lifestyles including golf, hiking, and recreational activities.
Regenerative medicine approaches including PRP and amniotic stem cell therapy can slow arthritis progression and improve function. For patients with mild to moderate joint degeneration, these treatments offer alternatives to joint replacement surgery.
Anti-inflammatory medication protocols account for summer dehydration risks. NSAIDs can affect kidney function, and dehydration compounds this risk. Arizona Pain and Spine Institute monitors kidney function and emphasizes hydration when prescribing NSAIDs during summer months.
Neuropathic Pain Conditions
Diabetic neuropathy, post-surgical nerve pain, and complex regional pain syndrome all involve nerve dysfunction causing burning, shooting, or electric-shock-like pain.
Medications modulating nerve function including gabapentin, pregabalin, and duloxetine form first-line pharmacological treatment. These work by changing how nerves generate and transmit pain signals.
Spinal cord stimulation provides advanced treatment options for patients with persistent neuropathic pain unresponsive to other interventions. The mild electrical signals from stimulator electrodes alter pain signal processing, significantly reducing pain intensity for many patients.
Arizona’s summer heat can worsen neuropathic pain for some patients. Treatment plans account for this by optimizing medication dosing before summer and ensuring patients have cooling strategies to prevent heat-related pain exacerbations.
Headaches and Migraines
Chronic headaches and migraines can be triggered by barometric pressure changes during Arizona’s monsoon season. Additionally, dehydration during summer months commonly causes or worsens headaches.
Preventive medications reduce headache frequency and severity. Options include certain antidepressants, anticonvulsants, and beta-blockers selected based on each patient’s headache characteristics and other health factors.
Nerve blocks targeting specific cranial nerves provide relief for certain headache types. Occipital nerve blocks help patients with occipital neuralgia or certain migraine patterns.
Hydration education is critical for Arizona headache patients. Many headaches result from inadequate fluid intake, especially during summer. Simple hydration improvements can dramatically reduce headache frequency.
When to Seek Specialized Pain Management in Arizona
Not all pain requires specialized care. However, certain circumstances indicate the need for pain management expertise.
Arizona Pain and Spine Institute recommends consultation when:
Pain persists beyond three months despite conservative treatment attempts. Chronic pain requires different approaches than acute injury pain.
Pain significantly limits daily activities, work capacity, or quality of life. When pain prevents you from doing things that matter, specialized intervention can help restore function.
Multiple treatment attempts with primary care providers haven’t produced adequate relief. Pain management specialists bring additional tools and expertise beyond general medical care.
Pain involves complex conditions like fibromyalgia, complex regional pain syndrome, or failed back surgery syndrome. These conditions require specialized knowledge for effective management.
Arizona’s seasonal changes predictably trigger pain flares. Recognizing patterns allows proactive treatment planning rather than reactive crisis management.
Pain affects mental health, causing depression, anxiety, or social isolation. The psychological impact of chronic pain deserves professional attention alongside physical treatment.
Arizona Pain and Spine Institute’s Commitment to Evidence-Based Care
Pain management advances rapidly as new research reveals more effective approaches. Arizona Pain and Spine Institute stays current with evolving evidence by following published clinical guidelines from leading organizations.
The practice incorporates recommendations from the 2022 CDC Clinical Practice Guideline emphasizing individualized, patient-centered decision-making. This means treatment plans reflect each patient’s unique circumstances, goals, and preferences rather than rigid protocols applied uniformly.
Following the 2024 American College of Occupational and Environmental Medicine (ACOEM) Chronic Pain Guidelines, Arizona Pain and Spine Institute tracks functional improvement as the primary treatment success marker. Rather than focusing solely on pain scores, physicians monitor increased physical capabilities, return to valued activities, exercise goal achievement, and overall quality of life improvements.
The 2023 WHO guideline on chronic low back pain reinforces non-pharmacological, non-surgical approaches as first-line treatment. Arizona Pain and Spine Institute follows this priority while ensuring patients have access to interventional and advanced options when conservative treatments prove insufficient.
Patient Success Through Arizona-Optimized Pain Management
Maria’s experience reflects how Arizona-optimized pain management transforms lives. After years of Minnesota winters leaving her arthritic knees aching, the warm, dry Arizona air provided immediate relief when she moved to Phoenix. However, her first Arizona summer brought unexpected challenges. The extreme heat increased inflammation, and summer dehydration worsened her pain despite the dry climate’s benefits.
At Arizona Pain and Spine Institute, Dr. Khan developed a comprehensive treatment plan accounting for seasonal variations. During winter and spring, Maria focused on outdoor walking and desert hiking to strengthen muscles supporting her knees. As summer approached, she transitioned to pool exercises at her community center, maintaining activity while staying cool.
Viscosupplementation injections before summer provided additional joint lubrication to handle increased activity during pleasant weather. A structured hydration protocol ensured adequate fluid intake during summer months. Anti-inflammatory nutrition strategies reduced systemic inflammation year-round.
The result was sustained improvement allowing Maria to enjoy Arizona living fully rather than simply surviving summers. Her pain remained manageable across seasons because treatment plans anticipated and addressed seasonal challenges proactively.
Conclusion
Pain management in Arizona requires understanding how the desert environment affects chronic pain conditions and implementing strategies that work with the climate rather than against it. Arizona Pain and Spine Institute brings specialized expertise in addressing the unique needs of Valley residents, from Cave Creek and Scottsdale to Phoenix and surrounding communities.
Effective pain management combines evidence-based medical treatment with Arizona-specific lifestyle adaptations. Whether addressing summer heat challenges, monsoon season pressure changes, or maximizing benefits from the dry climate, comprehensive approaches produce better outcomes than single-intervention treatments.
For Arizona residents living with chronic pain, specialized care that accounts for desert living makes the difference between merely coping and truly thriving. Arizona Pain and Spine Institute’s multimodal approach addresses pain from multiple angles while ensuring treatment plans fit how patients actually live in the Valley of the Sun.
Contact Arizona Pain and Spine Institute to schedule a comprehensive evaluation.

