Your knee hurts every morning when you step out of bed. Your doctor mentioned injections, but suddenly you’re facing four different options with wildly different prices and promises. At Arizona Pain and Spine Institute, Dr. Asim Khan sees this confusion daily. “Patients come in with printouts from the internet, stories from friends, and conflicting advice from different doctors,” he explains on the clinic’s website. “They need straight answers about what actually works.” This comparison breaks down exactly what each injection does, who benefits most, and what you can realistically expect.
Understanding What Goes Into Your Joint

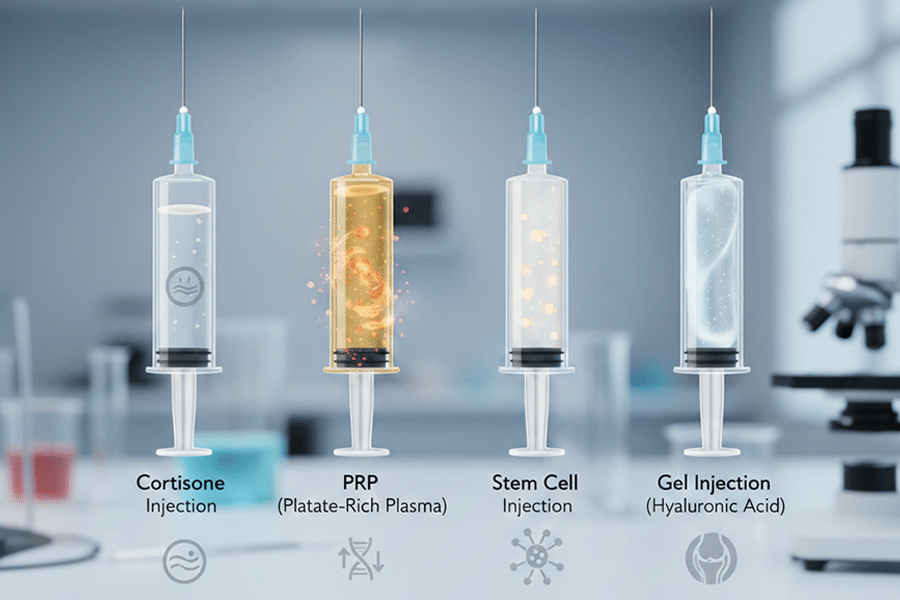
Before comparing these four treatments, it helps to understand what’s actually happening inside your painful joint. When you have arthritis, injury, or wear and tear, your joint becomes inflamed. The smooth cartilage that cushions bones gets rough or wears away. The fluid that lubricates the joint becomes thin and less protective. Your body’s healing systems can’t keep up with the damage.
Each injection type attacks these problems differently. Some calm inflammation quickly but temporarily. Others try to heal damaged tissue. Some simply add cushioning. Understanding these different approaches helps explain why your friend’s miracle injection might not work for you.
Cortisone Injections: The Quick Fix
Cortisone injections have been the go-to treatment for joint pain for over 50 years. Dr. Daniel Ryklin at Arizona Pain and Spine Institute explains that cortisone is a powerful anti-inflammatory medicine, similar to what your body naturally produces but much stronger. When injected directly into a painful joint, it rapidly reduces swelling and calms angry, inflamed tissue.
The process is straightforward and quick. At the Mesa or Gilbert offices of Arizona Pain and Spine Institute, the injection takes about five minutes. The doctor cleans the skin, numbs the area, and uses a thin needle to place the cortisone exactly where it’s needed. Many patients feel improvement within 48 hours, with maximum relief coming within a week.
Get Back Your Normal Life Again
As pain specialists, we can guarantee that we are more than qualified in alleviating your pain and treating your condition.
Here’s what makes cortisone attractive for many patients: insurance almost always covers it. The cost with insurance typically runs between $100 and $300 in copays. Even without insurance, cortisone injections at Arizona Pain and Spine Institute cost significantly less than other options, making them accessible for patients on tight budgets.
The relief from cortisone typically lasts three to four months, though this varies widely. Some patients get six months of relief while others only get six weeks. The injection works best for inflammatory conditions where swelling is the main problem. Patients with rheumatoid arthritis, acute injuries with swelling, or inflammatory osteoarthritis often see excellent results.
But cortisone has important limitations that Dr. Khan discusses with every patient. You can’t get these injections indefinitely. Most doctors limit patients to three or four per year because too much cortisone can actually weaken cartilage and surrounding tissues. Research published in the Journal of the American Medical Association shows that repeated cortisone injections may accelerate arthritis progression in some patients.
The other downside is that cortisone doesn’t fix anything. It’s like taking a very powerful, targeted anti-inflammatory pill. Once the medicine wears off, the underlying problem remains. For patients with mechanical problems or actual tissue damage, cortisone provides temporary relief but doesn’t address the root cause.
PRP: Your Body’s Own Healing Power
Platelet-rich plasma therapy represents a completely different philosophy from cortisone. Instead of suppressing inflammation with medication, PRP tries to accelerate your body’s natural healing processes. Dr. Khan has been performing PRP injections at Arizona Pain and Spine Institute since the clinic opened, with particular success in tendon injuries and mild to moderate arthritis.
The process starts with drawing your blood, about the same amount as a typical blood test. This blood goes into a special centrifuge that spins at high speed, separating the components. The platelets, which contain growth factors and healing proteins, get concentrated to levels five to ten times higher than normal blood. This golden-colored plasma is then injected back into your painful joint or injured tissue.
What happens next is fascinating biology. The concentrated platelets release growth factors that call in stem cells, stimulate new blood vessel formation, and accelerate tissue repair. It’s like sending a concentrated dose of your body’s repair crew directly to the problem area. Unlike cortisone, which works within days, PRP takes time. Patients typically start noticing improvement at three to four weeks, with maximum benefit at two to three months.
The research on PRP shows particularly good results for certain conditions. A study from the American Journal of Sports Medicine found that PRP outperformed cortisone for tennis elbow at six months and one year follow-up. For knee arthritis, patients with mild to moderate damage often see improvement lasting six to twelve months or longer.
Cost is where PRP becomes challenging for many patients. Insurance companies consider PRP experimental and won’t cover it, despite growing evidence of effectiveness. At Arizona Pain and Spine Institute, PRP treatments range from $1,500 to $4,000 depending on the area treated and the concentration protocol used. This upfront cost causes many patients to hesitate, though Dr. Ryklin points out that patients who respond well often save money long-term by avoiding repeated cortisone injections or surgery.
The ideal PRP candidate has mild to moderate arthritis or tendon injuries, is under 65 with good overall health, and wants to avoid or delay surgery. Patients with severe, bone-on-bone arthritis typically see limited benefit. The treatment also doesn’t work well for everyone—about 70% of appropriate candidates see significant improvement, meaning 30% don’t respond adequately.
Stem Cell Injections: Regeneration at the Cellular Level
Stem cell therapy takes regenerative medicine to its most advanced level. Arizona Pain and Spine Institute has offered amniotic stem cell therapy since 2016, making them one of the more experienced clinics in the Phoenix area. Dr. Khan emphasizes that these aren’t embryonic stem cells—they come from amniotic fluid donated during planned C-sections, avoiding ethical concerns while providing powerful regenerative potential.
The science behind stem cells is remarkable yet complex. These cells have the ability to transform into different types of tissue—cartilage, tendon, ligament, or muscle—depending on where they’re placed and what signals they receive. When injected into an arthritic knee, they can potentially regenerate worn cartilage. In a torn rotator cuff, they might help rebuild tendon tissue.
The procedure itself is simpler than PRP because the cells come prepared from an FDA-compliant tissue bank. There’s no blood draw or waiting for processing. Dr. Ryklin uses ultrasound or fluoroscopy (real-time X-ray) to guide the injection precisely where the cells are needed. The entire process takes about 30 minutes, though the preparation and explanation take longer than the actual injection.
What makes stem cells particularly exciting is their potential for actual tissue regeneration rather than just symptom management. Patients at Arizona Pain and Spine Institute have shown new cartilage growth on follow-up MRIs, something neither cortisone nor gel injections can achieve. The anti-inflammatory effects begin within days, but the regenerative process continues for months.
The timeline for stem cell therapy requires patience. Initial improvement might be noticed at two to four weeks as inflammation decreases. However, the real regenerative effects develop over three to six months. Some patients continue seeing improvement up to a year after injection as tissues rebuild and remodel.
Cost represents the biggest barrier for most patients considering stem cell therapy. Treatments at Arizona Pain and Spine Institute range from $15,000 to $25,000 depending on the number of joints treated and the concentration of cells used. Insurance doesn’t cover this treatment, and there are no guarantees of success. However, for patients facing joint replacement surgery, the investment might make sense if it delays or prevents a $50,000 operation.
The best candidates for stem cell therapy have moderate to severe arthritis but still have some joint space remaining, are younger than 75 with good healing capacity, have failed conservative treatments but want to avoid surgery, and can afford the treatment and understand it might not work. Dr. Khan reports that approximately 60-70% of properly selected patients see significant, lasting improvement.
Gel Injections: The Cushioning Approach
Gel injections, technically called viscosupplementation or hyaluronic acid injections, take yet another approach to joint pain. These injections don’t reduce inflammation like cortisone or promote healing like PRP and stem cells. Instead, they replace the natural lubricating fluid in your joint that has become thin and ineffective.
Think of your joint like a door hinge. When the hinge is well-oiled, it moves smoothly and quietly. When the oil dries up, it creaks and sticks. Gel injections essentially re-oil your joint with a synthetic version of the fluid that’s supposed to be there naturally. The gel is made from hyaluronic acid, a substance normally found in healthy joint fluid.
The treatment protocol varies depending on the specific product used. Some require a series of three to five weekly injections, while newer formulations work with a single injection. At Arizona Pain and Spine Institute, Dr. Ryklin typically uses single-injection formulas for patient convenience, though some insurance plans only cover the series versions.
The experience of getting gel injections is similar to cortisone—a quick, in-office procedure taking about ten minutes. The needle is slightly larger because the gel is thicker than other injections, but the discomfort is minimal. Unlike cortisone, you won’t feel rapid relief. The gel needs time to distribute through the joint and start providing cushioning. Most patients notice improvement at two to four weeks.
Insurance coverage for gel injections is inconsistent and often frustrating. Medicare and many insurance plans cover them for knee arthritis but not for other joints. Even for knees, insurers often require that you’ve failed other treatments first, including physical therapy and cortisone injections. The approval process can take weeks, during which you continue suffering.
When insurance does cover gel injections, your out-of-pocket cost might be $200 to $500 in copays for the series. Without insurance, the cost runs $2,000 to $4,000 for a full treatment series. This positions gel injections as a middle ground between cheap cortisone and expensive stem cells.
The effectiveness of gel injections remains controversial in medical literature. Some studies show benefit comparable to cortisone, lasting six months to a year. Other research suggests the benefit might be largely placebo effect. Dr. Khan’s experience at Arizona Pain and Spine Institute indicates that results vary dramatically between patients. Those with mild to moderate arthritis and good joint alignment tend to respond better than those with severe arthritis or mechanical problems.
Making Your Decision: Dr. Khan and Dr. Ryklin’s Framework

After treating thousands of patients with all four injection types, the physicians at Arizona Pain and Spine Institute have developed a practical framework for choosing the right injection. The decision depends on several factors that they evaluate during consultation.
The severity of your condition matters enormously. Mild inflammation responds well to cortisone. Mild to moderate arthritis might benefit from PRP or gel. Severe arthritis with significant tissue damage might require stem cells for any meaningful improvement. Dr. Ryklin uses imaging and physical examination to determine where you fall on this spectrum.
Your timeline affects the choice significantly. If you need relief for an event next week, cortisone is your only option that works quickly. If you can wait two to three months for improvement and want longer-lasting results, PRP or stem cells make more sense. Gel injections fall somewhere in between, taking a few weeks to work but not requiring the patience that regenerative treatments demand.
Financial reality can’t be ignored in medical decision-making. If insurance coverage is essential, cortisone and possibly gel injections are your options. If you can afford $1,500 to $4,000, PRP opens up as a possibility. Stem cells require significant financial resources or strong motivation to avoid surgery. Arizona Pain and Spine Institute offers payment plans for regenerative treatments, but the costs remain substantial.
Your overall health and healing capacity influence treatment success. Younger patients with good circulation and no chronic diseases often see better results from regenerative treatments. Older patients or those with diabetes, smoking history, or poor circulation might get more predictable results from cortisone or gel injections.
Previous treatment responses provide valuable information. If cortisone helped but didn’t last long enough, PRP might offer longer relief. If gel injections provided some benefit, stepping up to regenerative treatments might make sense. If nothing has helped, it’s important to reconsider the diagnosis before trying expensive treatments.
Combination Approaches: When One Isn’t Enough
Arizona Pain and Spine Institute often combines injection types for optimal results. Dr. Khan might use cortisone to quickly reduce inflammation, then follow with PRP once the acute swelling is controlled. This combination gives rapid relief while promoting longer-term healing.
Another common approach involves using PRP or stem cells for the primary problem area while using cortisone for secondary sites. For example, treating an arthritic knee with stem cells while using cortisone for associated hip bursitis that developed from limping. This targeted approach maximizes benefit while controlling costs.
The timing of combinations matters significantly. Cortisone can suppress the healing response triggered by PRP or stem cells if given too close together. The clinic typically waits at least six weeks between cortisone and regenerative treatments to avoid interference. This requires patience but optimizes outcomes.
Some patients benefit from alternating treatments. They might get PRP annually with cortisone injections as needed for flares. This approach provides a baseline of regenerative treatment with rescue therapy available for bad periods. It’s particularly useful for patients with progressive arthritis who want to delay surgery as long as possible.
Real Patient Experiences at Arizona Pain and Spine Institute
Understanding how these injections work in real life helps make better decisions. The clinic has treated thousands of patients with various injection types, providing insight into typical experiences and outcomes.
A 55-year-old teacher from Gilbert with moderate knee arthritis tried cortisone first. She got four months of excellent relief, then diminishing returns with repeated injections. After switching to PRP, she experienced six weeks of minimal improvement followed by progressive relief lasting over a year. She now gets PRP annually and remains active without surgery five years later.
A 67-year-old retired contractor from Mesa had severe shoulder arthritis from years of overhead work. Cortisone provided only two weeks of relief. Gel injections didn’t help at all. Despite the cost, he tried amniotic stem cells. Three months later, he had 60% improvement in pain and function. While not perfect, it allowed him to avoid shoulder replacement and maintain independence.
A 45-year-old marathon runner from Scottsdale developed severe knee pain from cartilage wear. Being young and active, Dr. Ryklin recommended PRP rather than cortisone to avoid potential cartilage weakening. After two PRP treatments six months apart, she returned to running and has maintained improvement for two years.
These examples illustrate that there’s no universal best injection. The right choice depends on individual circumstances, conditions, and goals. What works miraculously for one person might fail completely for another.
Conclusion
The great injection debate doesn’t have a simple winner. Each injection type has its place in treating joint and tissue pain. Cortisone provides rapid, affordable relief for inflammatory conditions but doesn’t last or heal tissue. PRP offers longer-lasting improvement and actual healing potential at moderate cost but takes time to work. Stem cells provide the greatest regenerative potential but require significant financial investment with no guarantee. Gel injections offer a middle ground for joint arthritis but with inconsistent results.
At Arizona Pain and Spine Institute, Dr. Khan and Dr. Ryklin help patients navigate these choices based on medical evidence, clinical experience, and individual circumstances. They don’t push expensive treatments when simpler options might work, but they also don’t let insurance limitations prevent discussion of potentially superior treatments.
The key is starting with proper diagnosis and realistic expectations. Schedule an evaluation at Arizona Pain and Spine Institute by calling (480) 986-7246 to discuss which injection type makes sense for your specific situation.
Frequently Asked Questions
Q: Which injection lasts the longest?
A: Stem cell therapy potentially provides the longest relief, sometimes permanent. PRP typically lasts 6-12 months, gel injections 6-9 months, and cortisone 3-4 months on average.
Q: Can I get different types of injections in the same joint?
A: Yes, but timing matters. Wait at least 6 weeks between cortisone and regenerative treatments. Dr. Khan can create a combination protocol.
Q: Why won’t insurance cover PRP if it works?
A: Insurance companies consider PRP experimental despite growing evidence. This classification allows them to exclude coverage regardless of effectiveness.
Q: How do I know if I’m a good candidate for stem cells?
A: Best candidates have moderate arthritis with some joint space remaining, good overall health, and have failed conservative treatments. Consultation determines candidacy.
Q: Are gel injections worth trying before surgery?
A: For knee arthritis, gel injections are reasonable to try, especially if insurance covers them. Response varies, but some patients get significant relief.
This article references information from Arizona Pain and Spine Institute, the American Academy of Orthopaedic Surgeons, the Arthritis Foundation, and peer-reviewed medical journals. Individual results vary based on condition severity, overall health, and treatment response. Consult with qualified healthcare providers for personalized treatment recommendations.