The International Association for the Study of Pain reports that between 10-40% of patients who undergo spine surgery continue to experience chronic pain despite technically successful procedures. At Arizona Pain and Spine Institute in Mesa and Gilbert, Dr. Asim Khan and Dr. Daniel Ryklin see these patients every week—individuals whose X-rays show perfect surgical results but whose pain has actually worsened since their operations.
Understanding Post-Surgical Pain Through Real Patient Experiences
Failed back surgery syndrome, despite its name, doesn’t always mean the surgery failed technically. The bones may fuse perfectly, the disc may be successfully removed, and the hardware properly placed, yet the patient experiences the same or worse pain than before the procedure. This paradox occurs because surgery addresses structural problems but can trigger new pain mechanisms that weren’t present before.
Arizona Pain and Spine Institute has treated hundreds of post-surgical patients since opening in 2016. Dr. Khan explains on the clinic’s website that post-surgical pain often stems from factors the original surgery couldn’t address. The surgery might decompress one nerve while scar tissue forms around another. It might stabilize one segment of the spine while placing excessive stress on adjacent segments. These secondary effects often don’t appear until months after the procedure, long after the surgeon has declared the operation successful.
The phenomenon of adjacent segment disease represents one of the most common complications following spinal fusion. When surgeons fuse two or more vertebrae together, those segments no longer move. The segments above and below must compensate for this lost motion, leading to accelerated degeneration. Research published in the Spine Journal indicates that adjacent segment disease occurs in approximately 25-30% of fusion patients within ten years, though symptoms often begin within the first year.
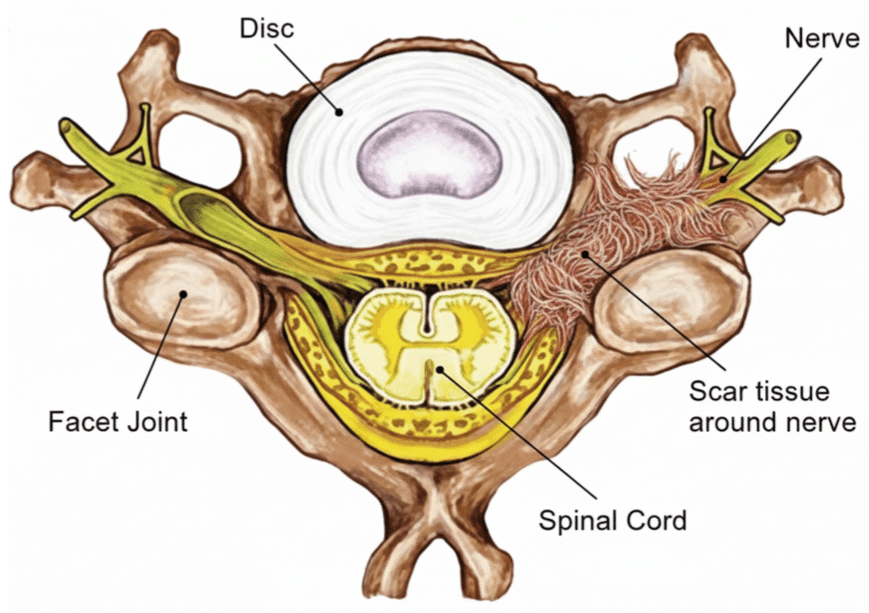
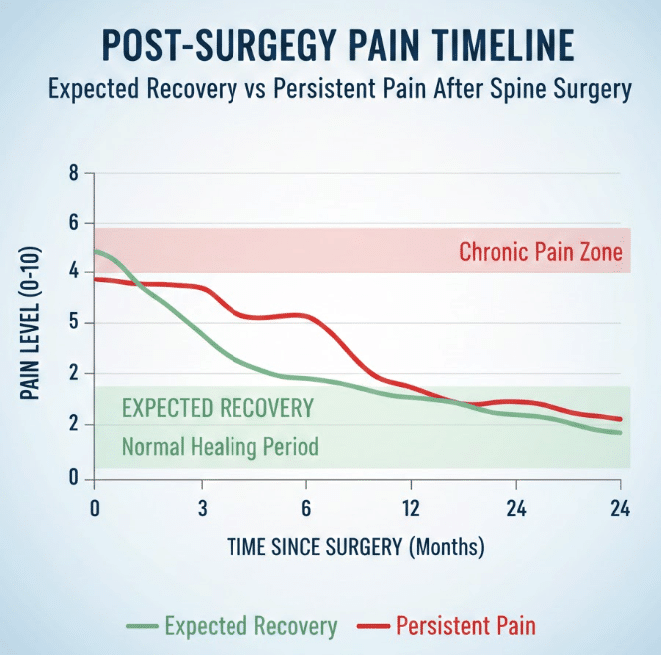
Scar tissue formation, medically termed epidural fibrosis, occurs in virtually all spine surgeries to some degree. While some scarring is normal and necessary for healing, excessive scar tissue can wrap around nerve roots, creating a new source of compression and pain. This scarring process continues for months after surgery, which explains why some patients feel improvement initially only to experience worsening pain three to six months post-operatively.
Get Back Your Normal Life Again
As pain specialists, we can guarantee that we are more than qualified in alleviating your pain and treating your condition.
The Biological Mechanisms Behind Persistent Post-Surgical Pain
The development of chronic pain after surgery involves complex biological processes that surgeons are only beginning to understand fully. Central sensitization, a process where the nervous system becomes hypersensitive to pain signals, can develop when pain persists beyond normal healing time. The Journal of Pain Research published findings showing that patients with pain lasting more than three months post-surgery show measurable changes in how their spinal cord and brain process pain signals.
Nerve damage during surgery, even microscopic injury not visible during the procedure, can lead to neuropathic pain that differs significantly from the original mechanical pain. This nerve-related pain often presents as burning, tingling, or electric shock sensations rather than the aching or stiffness typical of structural problems. The nervous system’s attempt to heal these microscopic injuries can result in abnormal nerve regeneration, creating pain signals where none should exist.
The inflammatory response to surgery extends far beyond the initial healing period. Research indicates that some patients maintain elevated inflammatory markers for months or even years after spine surgery. This chronic inflammation not only causes pain directly but also sensitizes surrounding nerves, making them more reactive to normal stimuli. Simple movements that shouldn’t cause pain become painful when tissues remain chronically inflamed.
Surgical alteration of biomechanics creates stress patterns the body isn’t designed to handle. When a surgeon removes a disc, fuses vertebrae, or implants hardware, the entire kinetic chain from the neck to the pelvis must adapt. These adaptations can strain muscles, ligaments, and joints that weren’t problematic before surgery. Physical therapy can help, but some biomechanical changes are permanent and continue generating pain signals.
How Arizona Pain and Spine Institute Approaches Post-Surgical Pain
The approach to treating post-surgical pain at Arizona Pain and Spine Institute begins with comprehensive pain evaluation to identify all pain generators, not just the original problem area. Dr. Ryklin, with his expertise in biomechanical assessment, examines how surgery has altered movement patterns and where new stress points have developed. This evaluation includes detailed imaging review, physical examination, and often diagnostic injections to pinpoint specific pain sources.
The clinic’s treatment philosophy for post-surgical patients emphasizes non-invasive interventions before considering revision surgery. As stated on their website, many patients who are told they need additional surgery can achieve significant improvement through targeted interventional procedures. This approach recognizes that additional surgery carries risks of creating more scar tissue and further altering biomechanics.
Spinal cord stimulation has emerged as a particularly effective option for failed back surgery syndrome. Arizona Pain and Spine Institute offers both traditional spinal cord stimulation and dorsal root ganglion stimulation, with Dr. Khan and Dr. Ryklin being among the few physicians in the Phoenix area trained in both technologies. The ability to trial the device before permanent implantation allows patients to experience the benefits without committing to another surgery. According to information on their treatment pages, many patients who felt hopeless after failed surgery find significant relief through neurostimulation.
Radiofrequency ablation can address pain from facet joints stressed by altered biomechanics after surgery. Since fusion surgery commonly leads to facet joint problems at adjacent levels, this treatment can provide months of relief without further surgery. The procedure targets specific nerves carrying pain signals from arthritic joints, essentially turning off the pain signal without affecting movement or strength.
The Role of Regenerative Medicine in Post-Surgical Healing
Regenerative medicine offers unique benefits for post-surgical patients that traditional treatments cannot provide. While Arizona Pain and Spine Institute has offered amniotic stem cell therapy since 2016, its application for post-surgical patients addresses the underlying tissue damage and chronic inflammation that perpetuates pain. The growth factors and anti-inflammatory properties of regenerative treatments can help normalize the inflammatory environment around surgical sites.
Platelet-rich plasma therapy, though not covered by insurance, provides concentrated healing factors directly to areas of persistent inflammation or incomplete healing. For post-surgical patients, PRP injections into areas of chronic inflammation or painful scar tissue can promote more normal healing patterns. The treatment doesn’t reverse surgery but can help tissues adapt better to their altered environment.
The timing of regenerative interventions matters significantly for post-surgical patients. Too early, and the normal healing process might be disrupted. Too late, and chronic changes become harder to reverse. The clinic’s experience suggests that the optimal window for regenerative treatments in post-surgical patients begins around six months after surgery, once initial healing is complete but before chronic pain patterns become fully established.
Psychological Factors in Post-Surgical Pain Persistence
The psychological impact of failed surgical outcomes cannot be overlooked in understanding persistent post-surgical pain. Patients who viewed surgery as their last hope often experience significant distress when pain persists or worsens. This emotional response isn’t just psychological suffering—it has real physiological effects that amplify pain perception.
Research published in Pain Medicine journal demonstrates that catastrophic thinking about pain, common in failed surgery patients, activates brain regions that intensify pain processing. The fear that nothing can help becomes a self-fulfilling prophecy as anxiety and depression lower pain thresholds and reduce the effectiveness of treatments. Arizona Pain and Spine Institute’s comprehensive approach includes addressing these psychological factors as part of the overall treatment plan.
The relationship between patient and surgeon after unsuccessful pain relief can become strained, with patients feeling abandoned when surgeons insist the operation was successful despite ongoing pain. This breakdown in the therapeutic relationship can delay appropriate treatment as patients struggle to find new providers willing to take on complex post-surgical cases. The clinic’s experience with these patients means they understand both the physical and emotional complexity of post-surgical pain.
Alternative Approaches and Combination Therapies

The most successful outcomes for post-surgical pain often come from combining multiple treatment modalities rather than seeking a single solution. Arizona Pain and Spine Institute’s approach typically involves addressing different aspects of pain simultaneously. Nerve pain might be treated with medication or stimulation while mechanical pain is addressed through injections or physical therapy.
Trigger point injections can provide relief for muscular pain that develops from compensatory movement patterns after surgery. When the body adjusts to surgical changes, certain muscles work harder than designed, developing painful trigger points. These injections not only relieve immediate pain but allow for more effective physical therapy to correct movement patterns.
The integration of physical therapy with interventional procedures improves outcomes significantly. However, standard physical therapy protocols often fail post-surgical patients because they don’t account for permanently altered anatomy. Specialized post-surgical rehabilitation focusing on working within new biomechanical constraints proves more effective than trying to restore pre-surgical movement patterns.
Medication management for post-surgical patients requires careful balancing. While the clinic emphasizes non-opioid approaches, appropriate medication can facilitate participation in physical therapy and other active treatments. The goal is using medication as a bridge to functional improvement rather than long-term management.
When to Seek Help for Persistent Post-Surgical Pain
Determining when post-surgical pain is abnormal rather than part of normal healing challenges both patients and providers. Generally, surgical pain should progressively improve after the first few weeks. Pain that worsens after initial improvement, develops new characteristics, or persists beyond three months warrants evaluation by pain specialists.
Warning signs that require immediate attention include new neurological symptoms such as weakness, numbness, or loss of bowel/bladder control. These symptoms might indicate hardware failure, infection, or new nerve compression requiring urgent intervention. However, most persistent post-surgical pain doesn’t represent an emergency but rather a complex pain syndrome requiring specialized management.
The timing of intervention for persistent post-surgical pain significantly impacts outcomes. Waiting too long allows central sensitization to develop and pain patterns to become entrenched. Early intervention, typically within six months of surgery if pain persists, provides the best opportunity for successful treatment. Arizona Pain and Spine Institute’s FastTrack program allows for rapid evaluation without the typical weeks-long wait for specialist appointments.
Realistic Expectations and Long-Term Management
Managing expectations is crucial for post-surgical pain patients. Complete pain elimination might not be realistic, but significant improvement in function and quality of life is achievable for most patients. The clinic’s treatment approach focuses on functional improvement rather than chasing zero pain, recognizing that some degree of discomfort might persist but shouldn’t prevent meaningful activities.
Long-term management of post-surgical pain often requires ongoing treatment rather than a one-time fix. Radiofrequency ablation might need repeating annually. Spinal cord stimulator settings might require adjustment as the body adapts. This ongoing management shouldn’t be viewed as treatment failure but rather as successful chronic disease management, similar to managing diabetes or hypertension.
The importance of lifestyle modifications in managing post-surgical pain cannot be overstated. Weight management reduces stress on surgical sites. Proper ergonomics prevents additional strain. Regular movement within safe parameters maintains flexibility and strength. These modifications work synergistically with medical treatments to optimize outcomes.
Conclusion
The persistence of pain after technically successful surgery represents one of the most frustrating experiences patients face. The expectation that surgery will solve the problem makes the reality of continued or worsened pain particularly difficult to accept. However, as Arizona Pain and Spine Institute demonstrates through their comprehensive approach to post-surgical pain, effective treatments exist that don’t require additional surgery.
Understanding that post-surgical pain often stems from new sources rather than surgical failure empowers patients to seek appropriate treatment rather than accepting suffering as inevitable. The combination of interventional procedures, regenerative medicine, and comprehensive pain management can provide relief even when surgery hasn’t delivered promised results.
For those living with persistent post-surgical pain, the next step is clear: schedule an evaluation with pain specialists experienced in managing failed back surgery syndrome and post-surgical pain conditions. Contact Arizona Pain and Spine Institute at (480) 986-7246 to discuss non-surgical options for managing post-surgical pain.
Frequently Asked Questions
Q: Why does my back hurt worse after successful surgery?
A: Surgery can trigger new pain sources including scar tissue formation, adjacent segment stress, and altered biomechanics that weren’t present before the procedure.
Q: How long should I wait before seeking help for post-surgical pain?
A: If pain persists or worsens beyond three months post-surgery, evaluation by a pain specialist is recommended to prevent chronic pain development.
Q: Can anything help if my fusion surgery didn’t relieve my pain?
A: Yes, treatments like spinal cord stimulation, radiofrequency ablation, and regenerative medicine can provide significant relief without additional surgery.
Q: Is it normal to have different pain after surgery than before?
A: Yes, post-surgical pain often has different characteristics due to nerve irritation, scar tissue, and biomechanical changes from the procedure.
Q: Should I consider revision surgery for persistent pain?
A: Non-surgical interventions should be tried first, as revision surgery carries risks of more scar tissue and potentially worse outcomes.
This article references publicly available information from Arizona Pain and Spine Institute, peer-reviewed medical journals including the Spine Journal, Journal of Pain Research, and Pain Medicine, and established medical literature on failed back surgery syndrome dated through 2024. All medical information reflects current understanding of post-surgical pain mechanisms. Results vary based on individual conditions, surgical procedures, and treatment responses. Consult qualified healthcare providers for personalized medical advice.

